Understanding Plaque Psoriasis: Essential Information
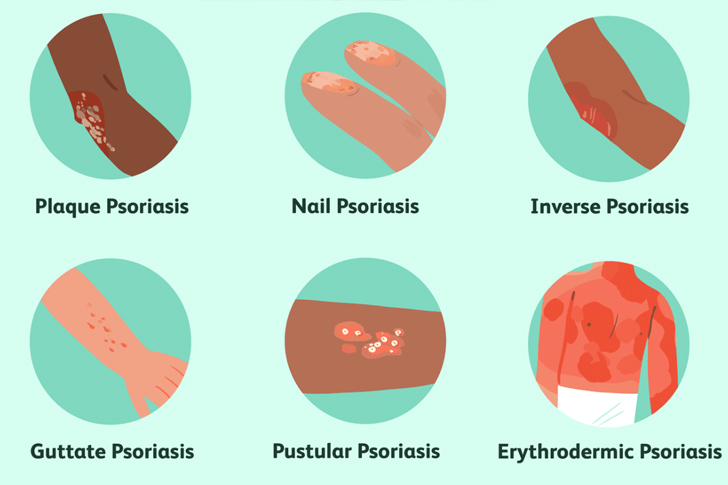
Plaque psoriasis is a chronic autoimmune condition characterized primarily by raised, red patches on the skin, which are typically covered with a silvery, scaly layer. This common form of psoriasis affects millions of people worldwide. To better understand this condition, it’s essential to explore its symptoms, causes, impact, and treatment options.
Symptoms and Diagnosis of Plaque Psoriasis
The most obvious symptoms of plaque psoriasis are the inflamed, red patches of skin, known medically as plaques, which commonly appear on the scalp, knees, elbows, and lower back. These plaques can be itchy and sometimes painful. During diagnosis, healthcare providers typically examine the affected skin and might take a small sample, or biopsy, to be certain that the diagnosis is correct, especially where the symptoms may be similar to those of other skin diseases.
Prevalence and Risk Factors
According to the World Health Organization, psoriasis affects more than 125 million people globally. Although plaque psoriasis can begin at any age, it often first appears between the ages of 15 and 25. Both genetic and environmental factors contribute to the development of the condition. Family history is a strong risk factor; having one parent with psoriasis increases your risk by 10%, which doubles if both parents have the condition. Other factors include stress, cold weather, smoking, and infections, particularly streptococcal infections.
Pathophysiology of Plaque Psoriasis
Psoriasis stems from an overactive immune system. Specifically, immune system cells called T cells mistakenly attack healthy skin cells, leading to an increased production of both skin cells and more T cells, leukocytes, and other markers of inflammation. This results in the faster turnover of skin cells, which accumulate on the skin’s surface as dead cells cannot be shed quickly enough, forming the characteristic scaly patches.
Impact on Quality of Life
The effects of plaque psoriasis extend beyond physical symptoms. Studies show that psoriasis is associated with significant mental and emotional distress and can dramatically decrease the quality of life. Patients with psoriasis are also at greater risk for co-morbid conditions such as cardiovascular diseases, psoriatic arthritis, type 2 diabetes, and depression. The stigmatizing visible aspects of the disease can also lead to low self-esteem and social isolation.
Treatment Options for Plaque Psoriasis
While there is no cure for plaque psoriasis, several treatments can help manage symptoms and improve the appearance of the skin. Topical treatments, such as corticosteroids and vitamin D analogues, are commonly used to reduce inflammation and slow down skin cell growth. For moderate to severe cases, phototherapy or systemic treatments, including biologics that target specific parts of the immune system, may be effective.
Recent Advances in Treatment
Recently, there has been significant progress in the treatment of plaque psoriasis. Newer biologic drugs are specifically designed to target the underlying immune pathways involved in psoriasis, offering more effectiveness and fewer side effects than traditional systemic therapies. The introduction of Janus kinase (JAK) inhibitors, for instance, has provided an alternative for those who cannot use biologics.
Living with Plaque Psoriasis
Living with plaque psoriasis requires more than just managing physical symptoms; it also involves addressing mental health and lifestyle changes. Stress management techniques, such as yoga and meditation, have proven beneficial. Additionally, a healthy diet and regular exercise can help manage not only the physical symptoms but also the associated risks of other conditions. Support groups and counseling can also play a crucial role in improving mental health and coping mechanisms.
The Future of Plaque Psoriasis Management
With ongoing research into the genetic and immunologic aspects of psoriasis, future treatments are likely to become even more personalized. This could potentially increase the efficacy of treatment regimens and offer new hope to those affected by the disease. Moreover, increasing public awareness and understanding of psoriasis, and dispelling myths and stigmas against the condition, are vital for improving the lives of those with psoriasis.
Understanding plaque psoriasis comprehensively involves recognizing its physical manifestations, underlying causes, psychological impacts, and the multi-faceted approaches required for effective management. Continued research and education are key to improving quality of life for those affected and potentially finding a cure.






Recent Comments